Make better informed cardiorespiratory decisions to improve patient outcomes
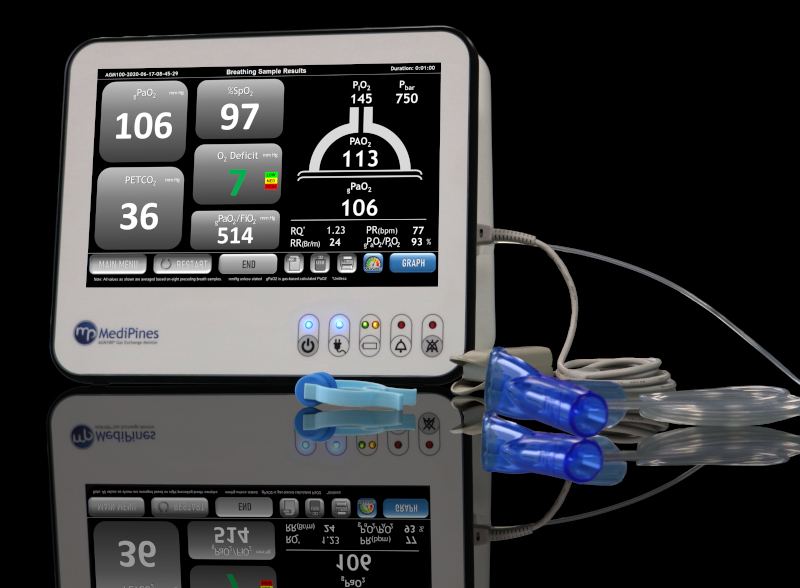
Experience enhanced decision-making capabilities with the AGM100 with instant access to crucial information on a patient's oxygenation, ventilatory status, and gas exchange impairment. This cutting-edge device empowers you to make the most informed clinical decisions possible.
Revolutionizing the way we comprehend oxygenation and respiratory impairment, the AGM100 provides multiple, real-time measurements to improve patient care.
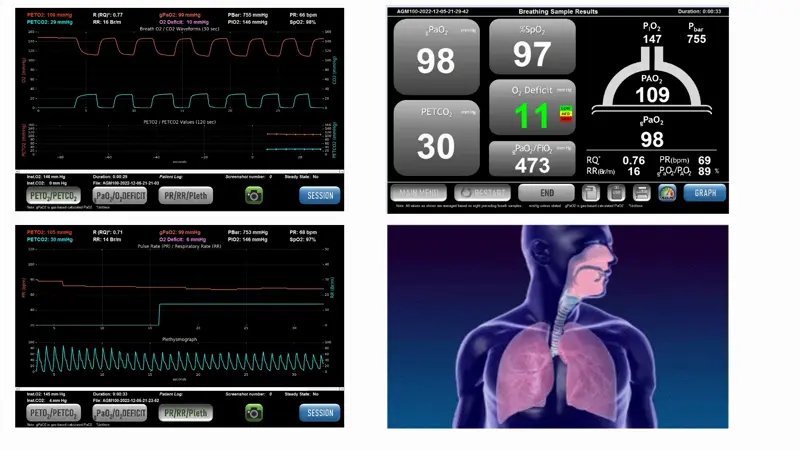
Identify the degree of respiratory impairment to improve clinical decision making
Pulmonary gas exchange in the alveoli is a vital process where blood exchanges carbon dioxide for oxygen. In the lungs, tiny air sacs called alveoli are surrounded by small blood vessels or capillaries. Oxygen-depleted blood, carrying carbon dioxide from the body, flows into these capillaries. Here, oxygen from the air in the alveoli moves into the blood, while carbon dioxide from the blood is released into the alveoli. This exchange happens through diffusion, where gases naturally move from an area of higher concentration to lower concentration. The refreshed, oxygen-rich blood then travels back to the heart to be circulated throughout the body, and carbon dioxide is exhaled from the lungs.
This process is essential for maintaining the balance of oxygen and carbon dioxide in our bodies. Our technology detects the levels of these gases (known as PO2 or PCO2) to detect abnormalities to help medical staff better assess patient’s impairment and overall cardiorespiratory health.
.png)
.png)
| Symbol | Description |
| gPaO2™ | Calculated arterial partial pressure of oxygen, mmHg |
| PETCO2 | End-tidal carbon dioxide partial pressure, mmHg |
| Oxygen Deficit | Gas exchange inefficiency (PAO2-gPaO2), mmHg |
| SpO2 | Blood oxygen saturation, % |
| Respiratory Rate (RR) | The number of breaths per minute |
| Pulse Rate (PR) |
The number of heart beats per minute |
| PAO2 | End-tidal oxygen partial pressure, mmHg |
| gPaO2/ FiO2 | Ratio of arterial partial pressure of oxygen to fraction of oxygen inspired |
| gPaO2/ PAO2 | Arterial to alveolar partial pressure of oxygen exchange ratio |
| RQ | Respiratory quotient, ratio of carbon dioxide produced to oxygen used |
| PiO2 | Partial pressure of inspired oxygen, mmHg |
| Pbar | Barometric pressure, mmHg |
Get the latest news on MediPines as we continue to advance respiratory medicine.